|
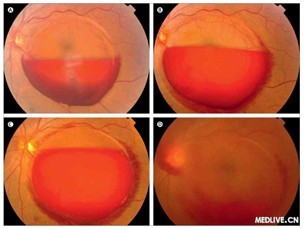
A和B 黄斑前内界膜下出血。C 随访期间血液沉积增加。D 14天后沉积的血液突破内界膜进入玻璃体凝胶。
Sub-inner limiting membrane haemorrhages
The Lancet, Early Online Publication, 15 March 2013
烟台毓璜顶医院 高磊,东长霞
2005年7月,一名47岁的男子因视力下降前来就诊。眼底镜检查显示,黄斑前内界膜下出血(图A)和内界膜的反光。随访中血液沉积逐渐增多(图B图C),并在14天后突破内界膜进入玻璃体凝胶(图D)。由于玻璃体出血稠密并且患者视物云雾感一直未消退,6周后行玻璃体切割术。术后视力改善。初步诊断Valsalva视网膜病变。内界膜下出血表现出后极部边界清晰、穹窿状出血,并导致严重的视力障碍。常与Valsalva 视网膜病变和Terson综合征有关。
In July, 2005, a 47-year-old man presented to us with impaired vision of his left eye. Fundoscopy examination showed premacular sub-inner limiting membrane haemorrhages (figure A) and a glistening light reflex reflected from the inner-limiting membrane overlying the haemorrhage. The sedimented blood increased during the follow-up period (figure B, C) and eventually broke through the inner-limiting membrane into the vitreous gel 14 days later (figure D). A vitrectomy was done because of the dense vitreous haemorrhage and his complaints of cloudy vision without spontaneous resolution after 6 weeks. Postoperative vision improved. A tentative diagnosis of Valsalva retinopathy was made. Sub-inner limiting membrane haemorrhages appear as sharply demarcated, dome-shaped haemorrhages at the posterior pole and consequently lead to severe visual impairment. They have been reported in association with Valsalva retinopathy and Terson's syndrome.
|